53% Improvement in RCM Productivity in Less Than 100 Days
The Challenge
Great Lakes Dental Partners (GLDP) is a dental support organization (DSO) committed to offering dentists and dental specialists the opportunity to focus on the clinical aspects of dentistry, providing exceptional care for every patient. GLDP is dedicated to advancing dental healthcare in the Midwest and has grown rapidly over the past two years to over 40 partner locations.
The DSO’s growth has resulted in different and fragmented revenue cycle management (RCM) processes across partner locations. Each affiliation brought with it a different approach to revenue cycle management. GLDP inherited processes ranging from in-house RCM, to outsourcing, to decentralized teams.
Managing so many different approaches to the same function became time-consuming and increasingly complex. The lack of centralization also created a data and reporting disconnect, making it difficult for GLDP management to accurately assess performance across insurance billing, revenue, and payer operations. Legacy RCM processes also translated into significantly higher costs for GLDP than an otherwise centralized billing office would benchmark for DSOs.
The Opportunity
As part of their integration strategy for new partner locations, GLDP had plans to overhaul the RCM function to improve process efficiency and revenue outcomes.
Donna Ramadan GLDP’s Director of Revenue Cycle, shared that:
Through our research and planning, we learned that the state of the market for end-to-end dental insurance RCM solutions is poor. We realized we had to approach our strategy one challenge at a time, staging each solution separately. The Remit AI software from Zentist stood out as an impactful yet targeted solution that aligned with our approach.
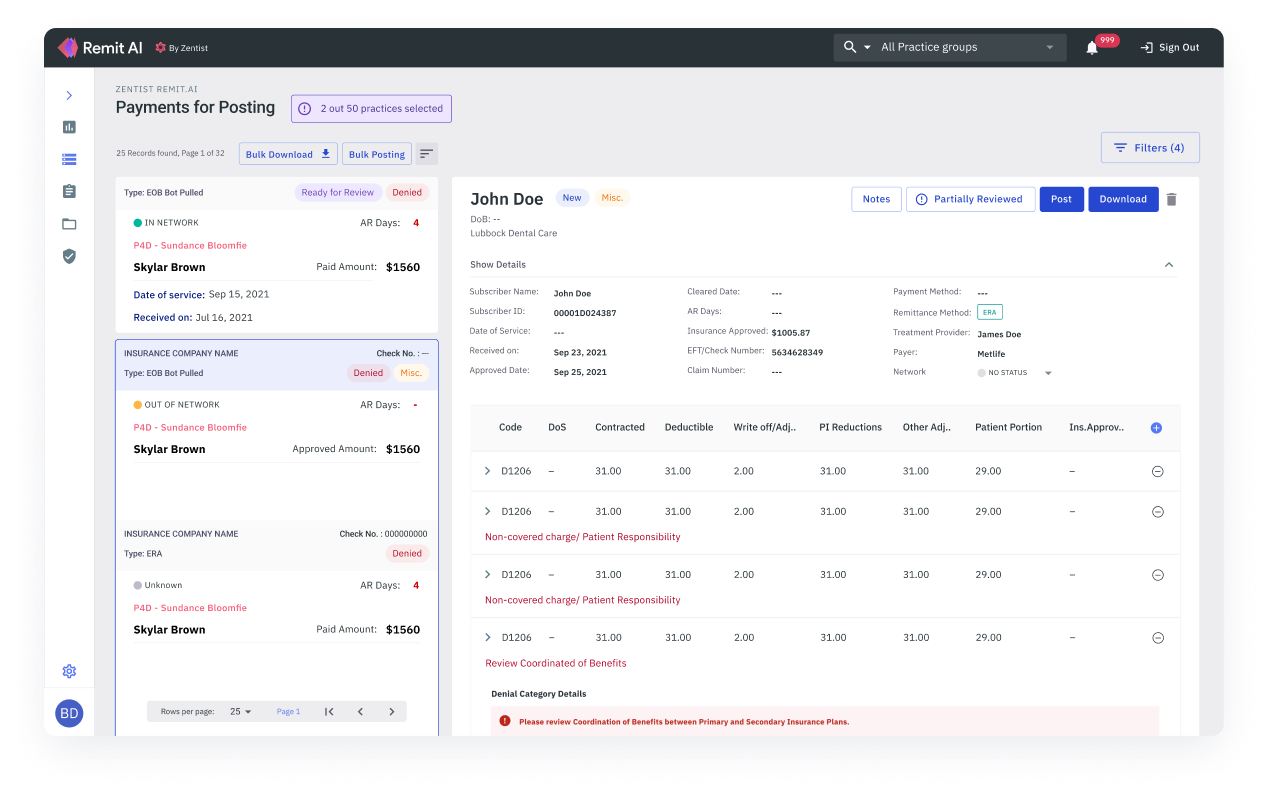
To validate earlier and faster results, GLDP began with a limited implementation across 5 partner locations. Within 40 days GLDP was able to see the meaningful impact of the Remit AI platform in areas such as automatic generation of explanation of benefits (EOB) and electronic remittance advice (ERA) data and automatic triaging of claims denials. As a result, GLDP was able to plan out and implement two key adjacent software components, Remit AI and PMS Posting Writeback across all partner locations.
The Outcome
As of today, less than 100 days since full deployment of Remit AI + PMS Posting Writeback, the following outcomes have been achieved:
The secret to GLDP’s success has been their pragmatic approach to what selective RCM processes should be and can be automated today with real efficiency and financial goals in mind.GLDP’s initial research and thoughtful planning allowed them to leverage modern technologies to age old problems in a targeted way, and that has opened up further automation opportunities moving forward.
With the current automation levels achieved, we are so much better equipped to deliver strategic value to the dentists who have partnered with GLDP. We are now working with Zentist to modernize the claims scrubbing and submission process.
Try Zentist Cloud-based RCM Dental Solution Now.
Schedule a free demo